Rapid Action Drug Alerts and Response (RADAR) quarterly report
January 2023
- Published
- 24 January 2023
- Type
- Statistical report
- Author
- Public Health Scotland
- Topics
-
Drugs
About this release
Our quarterly report
The Drugs Team at Public Health Scotland (PHS) has compiled this report of drug-related indicators in order to inform action to prevent drug harms and deaths.
The objectives of this report are to:
- monitor changes in drug trends, harms and use of services to inform immediate and short-term actions that reduce drug harms
- detect potential clusters of harms and recommend appropriate responses
Update
This publication was updated on 26 January 2023, with a slight amendment to provide the total figures for October 2022 in the suspected drug deaths indicator.
There was a minor update to this publication on 27 July 2023, in the opioid substitution therapy indicator. The glossary was updated to state that injectable buprenorphine is administered as a subcutaneous injection (previously listed as an intramuscular injection).
Data and reporting period
- Observed changes in indicators may reflect genuine trends in behaviours but may also be influenced by factors such as the configuration of services, or data quality and completeness issues.
- This release reports on Scotland-level data. Analysis for some indicators is available by NHS Board in the substance use section of the COVID-19 wider impacts dashboard.
- These data may be subject to change. Further analysis of these data will be made available in our Official and National Statistics publications on substance use.
- Different time periods may be reported across the different indicators. In all cases, the most recently available data are used. Most charts are based upon a 2-year time series.
- Key time periods, during which notable pandemic restrictions were in place, are indicated by reference lines and shaded areas on the charts. For more information on COVID-19 restrictions, view this timeline from the Scottish Parliament Information Centre.
Date of next report
The next release of this publication will be 25 April 2023.
Acknowledgements
This report reflects the collective efforts of different organisations and hundreds of people in frontline and supporting roles who record, organise, analyse and interpret information from a range of sources and services.
We gratefully acknowledge the continued commitment and effort of all those involved.
Summary of indicators
- Police Scotland drug trends bulletin
This update provides information on street benzos (benzodiazepines) and nitazenes mis-sold as oxycodone.
- Reports of drug harms to RADAR
18 reports were validated by RADAR between 24 September 2022 and 11 January 2023.
- Naloxone administration by Scottish Ambulance Service
The number of incidents between September and November 2022 (832) were lower compared to the same time period in 2020 (1,032) and 2021 (1,176).
- Drug-related attendances at emergency departments
The number of attendances between September to November 2022 (1,022) were slightly lower than expected for this time period comparing to similar time periods in the previous two years (1,068 attendances in 2021 and 1,114 in 2020).
- Drug-related acute hospital admissions
The number of admissions between July and September 2022 (2,024) were considerably lower compared to the same time period in 2020 (3,643) and 2021 (3,033).
- Suspected drug deaths
The average weekly number of suspected drug deaths increased in October and November 2022, following a decreasing trend in recent months. There were 76 suspected drug deaths in October 2022 and 109 suspected drug deaths in November 2022. The number of suspected drug deaths in November 2022 (109) was 17% higher than in November 2020 (93) and 22% higher than in November 2021 (89).
- Emergency department toxicology: ASSIST
Between August and November 2022, 169 detections of 30 different illicit drugs were identified by the ASSIST pilot. More than one substance was detected in 82% of attendances.
- Forensic toxicology testing for controlled substances
During July to September 2022, the most commonly found drugs or drug types in post-mortem testing were opioids (74%) and benzodiazepines (50%). Heroin/morphine was detected in 35% of deaths and there was a continued reduction in detections for etizolam (17%) and methadone (25%).
- Drug seizures in Scottish prisons
Synthetic cannabinoids were the most prevalent drug type detected in drug seizures in Scottish prisons during April, detected in 50% of samples. In contrast, benzodiazepines were the most prevalent in May, detected in 27% of samples.
- Specialist drug treatment referrals
The number of specialist drug treatment referrals between August to November 2022 (4,620) were lower compared to the same time periods in 2020 (5,092) and 2021 (5,511).
- Opioid substitution therapy
The average number of opioid substitution therapy (OST) doses supplied per month decreased slightly in the period from July to September 2022. The number of OST doses supplied during this period was higher than in the same time period in 2018 and 2019, and lower than in the same time period in 2020 and 2021.
- Injecting equipment provision
The average weekly numbers of Injecting Equipment Provision (IEP) transactions, and needles and syringes distributed were broadly stable between July and September 2022. The total numbers of IEP transactions, and needles and syringes distributed during this time period were lower compared to the same time periods in 2020 and 2021.
Main points
- An increase in suspected drug deaths was observed in Scotland between October and November 2022. All other healthcare indicators of harm and service utilisation remained stable and below expected levels. The predominant picture of drugs harms in Scotland continues to be polydrug use involving benzodiazepines, stimulants and opioids. Partners are advised to strengthen harm reduction and support measures with particular consideration for those who may have limited contact with health and social care services.
- This report also contains an alert on nitazene-type opioids in Scotland, which requires action by people working and volunteering in drug and alcohol services, emergency services, health care settings and high-risk settings.
Alerts
- RADAR has published a public health alert called nitazene-type opioids in Scotland. This is in response to an increase in the availability of a new group of synthetic opioid drugs called nitazenes.
- Due to their unexpected presence in the drug supply and high potency, nitazenes pose a substantial risk of overdose, drug-related hospitalisation and drug-related death.
- This alert details the action required by people working and volunteering in drug and alcohol services, emergency services, health care and medical settings and high-risk settings, such as prisons and hostels.
- Actions required include sharing harm reduction information, promoting naloxone distribution and increasing awareness of the signs of an overdose.
Trends
- 18 reports were validated by RADAR between 24 September 2022 and 11 January 2023.
- Benzodiazepines were the most commonly reported drug type, with seven (39%) reports indicating a benzodiazepine as the ‘primary drug’. Three reports related to bromazolam. Bromazolam is a Class C benzodiazepine that is structurally similar to alprazolam.
- There were also seven reports where a stimulant was reported to be the ‘primary drug’. Four reports were about the adverse effects of both cocaine powder and crack cocaine.
- Half of reports mention mixing two or more substances (polydrug use). Mixing drugs can cause unexpected and unpredictable effects and is a major risk factor in drug-related deaths in Scotland.
Harm indicators
- Scottish Ambulance Service naloxone incidents between September and November 2022 (832) were lower compared to the same time period in 2020 (1,032) and 2021 (1,176).
- The number of drug-related hospital admissions between July and September 2022 (2,024) were considerably lower compared to the same time period in 2020 (3,643) and 2021 (3,033).
- Suspected drug deaths increased in October and November 2022, following a decreasing trend in recent months. There were 109 suspected drug deaths in November 2022. This is higher than in the same month in 2020 (93) and 2021 (89).
Toxicology indicators
- In the ASSIST hospital toxicology pilot, two or more substances were detected in 82% of drug-related emergency department presentations. The most commonly detected drug was cocaine (13%), followed by desmethyldiazepam (11%) and cannabis (9%).
- Changes were observed in post-mortem toxicology in quarter 3 of 2022, with the percentage of cases testing positive for etizolam (17%) falling below diazepam (24%) for the first time since before 2019. The most commonly detected drug type in post-mortem testing was opioids (74%). Heroin/morphine was detected in 35% of deaths.
- Prison drug analysis also shows a changing picture of drug use as new synthetic cannabinoids and benzodiazepines continue to appear. Synthetic cannabinoids were the most commonly detected drug type in April 2022, detected in 50% of samples. In contrast, benzodiazepines were the most common in May 2022, detected in 27% of samples.
- The constant evolution in the types of substances available emphasises the importance of investment in drug checking, forensic post-mortem toxicology and hospital toxicology testing.
Service indicators
- The number of specialist drug treatment referrals between August and November 2022 were lower compared to the same time periods in 2020 and 2021.
- The average number of opioid substitution therapy doses supplied per month decreased slightly in the period from July to September 2022. The number of doses supplied during this period was higher than in the same time period in 2018 and 2019, and lower than in the same time period in 2020 and 2021.
- The average weekly number of injecting equipment provision transactions, and needles and syringes were broadly stable between July and September 2022. The total numbers of transactions and needles and syringes distributed during this time period were lower compared to the same time periods in 2020 and 2021.
Alerts
RADAR publishes ad-hoc alerts related to new drugs, trends and harms.
A public health alert about nitazene-type drugs in Scotland, was published on 24 January 2023.
This alert relates to an increase in the availability of a new group of drugs called nitazenes.
Nitazenes are potent synthetic opioids. Due to their unexpected presence in the drug supply and high potency, nitazenes pose a substantial risk of overdose, drug-related hospitalisation and drug-related death.
Trends
Police Scotland drug trends bulletin
This bulletin contains photos of drugs.
This update provides information on street benzos (benzodiazepines) and nitazenes mis-sold as oxycodone.
This information has been provided by Police Scotland’s STOP Unit to raise awareness of drug appearance and to demonstrate some of the substances present in Scotland’s drugs market.
Street benzos
'Street benzos' is a term used to describe benzodiazepines that are unlicensed or illicitly produced.
Most common benzodiazepines
- Etizolam is the most common active ingredient used to produce these tablets, but an increasing number of new benzodiazepine types and forms continue to appear.
- White ‘10’ with a half score on the reverse is still the most commonly recovered illicitly produced street benzodiazepine tablet.
- Light blue ‘D/10’ with a half score on the reverse is the second most commonly recovered street benzodiazepine tablet.
Flubromazepam
Flubromazepam is a Class C drug. Some recent recoveries of note are the following tablets:
- A white tablet with what appears to be a back to front ‘10’, with a half score on the reverse, containing flubromazepam.

- A light blue tablet ‘V10’ with a half score on the reverse, containing flubromazepam.

Bromazolam
There has been a recent increase in the number of bromazolam recoveries across Scotland. Bromazolam is a Class C drug.
According to recent information shared by the Scottish Prison Service, bromazolam has been detected in prisons in tablet and powder form. Reports suggest a link between the use of powder (suspected to be bromazolam) and serious and adverse health effects. The intelligence indicates that it is being obtained in pure powder form and consumed per ‘grain’.
A bulletin issued by Northumbria Police in June 2022 shows bromazolam was detected within ‘benzo bear’ jelly sweets, but no such recoveries have been found in Scotland at this time.

Visit NHS inform for more information on benzodiazepines.
Oxycodone/nitazene tablets
A recovery in Aberdeen found a quantity of tablets bearing oxycodone markings that contained N-pyrrolidino etonitazene, a highly potent opioid.
Oxycodone is available on prescription in the UK and is a Class A controlled drug within the provisions of the Misuse of Drugs Act 1971.
N-pyrrolidino etonitazene is not yet classified under the Misuse of Drugs Act 1971, but recommendations have been made to the Home Office that this drug and other similar synthetic opioids should be classified as Class A in the future.
For more information on this recovery, see the Police Scotland interim drug bulletin (10 November 2022).
For more information on nitazenes, see the nitazene-type drugs in Scotland RADAR alert.
Additional information
This information is provided to PHS by Police Scotland.
Reports of drug harms to RADAR
18 reports were validated by RADAR between 24 September 2022 and 11 January 2023.
A summary of validated reports is shown below for informational purposes.
These were received through our online reporting form and mailbox.
These reports have been collected as part of intelligence gathering.
PHS recommends the widespread use of the following harm reduction messages and interventions across Scotland.
Be cautious
Drugs in circulation can vary widely
- The drug purchased may not always be the drug that it’s expected to be.
- It may contain adulterants, be mis-sold or contain a different amount than anticipated.
Test before use
- Drug contents cannot be confirmed by the way it looks, smells or tastes.
- People in Scotland can get their drugs tested by using the free, anonymous postal service provided by WEDINOS.
Mixing drugs is dangerous and should be avoided
- Mixing drugs increases the risk of drug harms and death – this includes mixing alcohol with other drugs.
- Those taking medicines should research any potential interactions between their medicines and the drugs they are taking.
- The risk of overdose is also increased if someone takes drugs alone, takes drugs after a break, takes higher purity drugs than expected or injects drugs.
Get help in an emergency
- If someone needs medical help, call 999, ask for an ambulance and stay with the person until help arrives.
- If the person is non-responsive and displaying the signs of an overdose (unconsciousness, shallow breathing, snoring, blue lips, pale skin, pin-point pupils), administer naloxone.
Be informed
General drug information
Harm reduction information
Technical or scientific information
East Scotland
Report 1
- Local authority
City of Edinburgh
- Reason for report
New trend
- Drug
Mephedrone
- Appearance
Unknown
- Summary
Reports of heroin and cocaine suspected to be cut with mephedrone ('magic') causing adverse effects including heart palpitations.
Report 4
- Local authority
City of Edinburgh
- Reason for report
New trend, adverse effects
- Drug
Pregabalin
- Appearance
Red and white capsule with '300' or signature written on it
- Summary
Drug sold as pregabalin (suspected to be fake) causing adverse effects
Report 6
- Local authority
City of Edinburgh
- Reason for report
Adverse effects, new trend
- Drug
Valium
- Appearance
White tablets, 'KB10' on one side
- Summary
Bough as Valium and described as a cheaper and stronger alternative to 'ROCHE 10' tablets. Adverse effects include feeling unwell.
Report 8
- Local authority
West Lothian
- Reason for report
Adverse effects
- Drug
Cocaine
- Appearance
Unknown
- Summary
Report of three separate incidents involving different patients across a similar time period. All experienced side effects after snorting cocaine powder. Two patients reported the use of alcohol. Adverse effects include: chest pain, confusion, elevated pulse, hand cramping, hyperthermia, nausea/vomiting, respiratory arrest and seizures.
Report 10
- Local authority
Fife
- Reason for report
Adverse effects
- Drug
Ketamine
- Appearance
Unknown
- Summary
Serious, unexpected adverse effects including amnesia and seizures.
Report 11
- Local authority
Fife
- Reason for report
New drug
- Drug
Combination
- Appearance
Unknown
- Summary
Client’s report taking ‘double cap boosters’ to enhance the effect of street valium. Reports suggest benzos are taken alongside two prescription-only medicines, one anticonvulsant medication used in the treatment of epilepsy, and one antispasmodic medication used as a muscle relaxer.
Report 14
- Local authority
City of Edinburgh
- Reason for report
Adverse effects
- Drug
Cocaine
- Appearance
Yellow crystal
- Summary
Reports crack cocaine is suspected to be cut with mephedrone causing adverse effects including coughing up blood.
Report 15
- Local authority
Scottish Borders
- Reason for report
New drug
- Drug
Bromazolam
- Appearance
Tablet
- Summary
Bromazolam detected by WEDINOS in drug sold as diazepam.
Report 17
- Local authority
Fife
- Reason for report
New drug
- Drug
Bromazolam
- Appearance
Tablet
- Summary
Four samples were sent to WEDINOS, all sold as diazepam. The two white tablets contained etizolam, the two blue tablets contained bromazolam.
West Scotland
Report 13
- Local authority
North Lanarkshire
- Reason for report
New trend
- Drug
Methamphetamine
- Appearance
Unknown
- Summary
Three separate reports from services about the recent use of methamphetamine by clients.
Report 16
- Local authority
North Lanarkshire
- Reasons for report
Adverse effects
- Drug
Cocaine
- Appearance
Unknown
- Summary
Report of three patients, with no known links, admitted to hospital in one weekend after taking cocaine. One patient reported polydrug use. One patient had a cardiac arrest, two had seizures.
Report 18
- Local authority
NHS Lanarkshire (North Lanarkshire and South Lanarkshire)
- Reason for report
Adverse effects
- Drug
Cocaine
- Appearance
Unknown
- Summary
Increase in patients presenting to ear, nose and throat doctors with severe nose damage due to cocaine use. The cocaine causes severe inflammation and often leads to the wall between the nostrils collapsing. Other adverse effects include pain, malaise and fatigue. This effect seems to be worse in patients who also test positive for levamisole (cutting agent).
North Scotland
Report 2
- Local authority
Aberdeen City
- Reason for report
Adverse effects, withdrawal
- Drug
Temazepam
- Appearance
White tablets
- Summary
Service supporting patient withdrawing from 40 mg daily dose of temazepam after their prescription became unavailable due to shortages. Adverse effects from cessation of temazepam included anxiety/panic, confusion, decreased energy, depression/low mood, hallucinations, nausea/vomiting and suicidal thoughts/ideation.
Report 3
- Local authority
Aberdeenshire
- Reason for report
Concern - increased availability and use
- Drug
Mephedrone
- Appearance
Cream/white crystal
- Summary
Increase in the use of mephedrone (mcat) amongst young people. Reports of exploitation of young people with sales pushed by dealers and on social media for £25 per bag. Effects include anxiety/panic and increased energy. Presence of mephedrone confirmed by police testing, WEDINOS and testing kits.
Report 5
- Local authority
Aberdeenshire and Aberdeen City
- Reason for report
Adverse effects, overdose
- Drug
Valium
- Appearance
White tablet, '10' on one side
- Summary
Overdose (unconsciousness) after taking crack cocaine, methadone and a drug sold as Valium (bought from a dealer for £1 per pill). Hospital toxicology screen was negative for benzodiazepines.
Report 7
- Local authority
NHS Grampian (Aberdeen City, Aberdeenshire, Moray)
- Reason for report
Alert
- Drug
Promethazine
- Appearance
Syrup
- Summary
Alert after a recent increase in requests for promethazine (antihistamine) in Grampian community pharmacies, suspected to be related to the manufacture of lean. Lean is the name of a syrup/liquid taken for psychoactive effects, made by combining codeine (opioid), antihistamines and sweet/fizzy drinks.
Report 9
- Local authority
Aberdeenshire
- Reason for report
New trend
- Drug
Bromazolam
- Appearance
Blue bar
- Summary
Bromazolam detected by WEDINOS in drug sold as Xanax, purchased from dealer for £1 per bar. Adverse effects include amnesia and decreased energy. Taken alongside crack cocaine, other benzodiazepines, methadone and image and performance enhancing drugs (IPEDs).
Report 12
- Local authority
Aberdeen City
- Reason for report
Alert, new drug
- Drug
N-pyrrolidino etonitazene
- Appearance
Blue tablets, 'M' on one side, half score and '30' on the other
- Summary
A recent recovery of a quantity of tablets bearing oxycodone markings were found in the Aberdeen area and on examination, found to contain N-pyrrolidino etonitazene.
Reporting drug harms
Share information on trends, incidents and harms related to drugs, such as:
- adverse effects
- routes of administration
- testing data
Make a report by using our reporting form or by emailing phs.drugsradar@phs.scot
Harm indicators
Naloxone administration by Scottish Ambulance Service
The average weekly number of naloxone administration incidents was broadly stable between September and November 2022 (69 incidents per week). The total number of incidents during this time period (832) was lower compared to the same time periods in 2020 (1,032) and 2021 (1,176).
Background
Naloxone is a medicine used to prevent fatal opioid overdoses. These data relate to the number of incidents in which naloxone was administered by Scottish Ambulance Service (SAS) clinicians.
While these data count multiple overdose patients at the same incident separately, multiple naloxone administrations to the same patient at the same incident are not counted separately.
The chart below shows the weekly number of SAS naloxone administration incidents from 31 August 2020 to 27 November 2022.
Summary
Historic trend
- Until winter 2021, the average weekly number of SAS naloxone administration incidents was similar to previous years, which have generally been characterised by lower numbers of incidents during winter months and higher numbers during summer months.
- In spring 2022, the trend diverged from previous years and, in spite of an increase in April, the number of naloxone incidents has remained relatively stable since January 2022. At the end of May 2022, the number of naloxone incidents was approximately 25% lower compared to the same time period in 2021.
Update
For the most recent time period (5 September to 27 November 2022):
- 832 SAS naloxone incidents were recorded, at an average of 69 per week. Weekly numbers of incidents were generally stable throughout this period.
- The total number of incidents was 8% lower than in the previous 12-week time period (13 June to 4 September 2022) when 904 incidents were recorded, at an average of 75 per week.
- The total number of incidents was 19% lower than expected compared to the same time period in 2020 (1,032 attendances, average of 86 per week) and 29% lower than in 2021 (1,176 attendances, average of 98 per week).
Additional information
PHS was provided with these data by SAS.
For more information, or to analyse this data by NHS board, visit the COVID-19 wider impacts dashboard.
Why we use a 3-week moving average
As these data are highly variable over time, a 3-week moving average has been included in the graph to aid interpretation of trends over time.
Scotland’s Take-Home Naloxone Programme
The Take-Home Naloxone Programme was launched by the Scottish Government in 2011 to prevent fatal opioid overdoses.
Naloxone is a medicine that can temporarily reverse the effects of an opioid overdose. It can be given to anyone who is non-responsive and displaying the signs of an overdose (unconsciousness, shallow breathing, snoring, blue lips, pale skin, pin-point pupils).
Anyone in Scotland can carry naloxone. It can be accessed through most local drug services or pharmacies and it can also be delivered to your home through the charity Scottish Families Affected by Alcohol and Drugs.
Naloxone is very easy to administer.
You can learn more about administering naloxone in a free e-learning module created by the Scottish Drugs Forum.
Information on Take-Home Naloxone distribution can be found in the substance use section of the COVID-19 wider impacts dashboard and in the National Naloxone Programme Scotland Quarterly Monitoring Bulletin, both published by PHS.
Drug-related attendances at emergency departments
Average attendances were stable between September and November 2022 (1,022 attendances). Number of attendances were slightly lower than expected for this time period comparing to similar time periods in the previous two years (1,068 attendances in 2021 and 1,114 in 2020).
Background
A drug-related emergency department (ED) attendance is an attendance for a drug intoxication or overdose, either alone, or combined with alcohol intoxication.
The chart below shows the weekly number of drug-related ED attendances between 2 November 2020 and 27 November 2022.
Summary
Historic trend
- An overall decreasing trend was observed in drug-related attendances at EDs between August 2021 and April 2022, with the lowest weekly levels in the time series observed in the week beginning 4 April 2022 (54).
- Drug-related ED attendances then increased sharply and peaked in May 2022, with the highest weekly levels in the time series observed in the week beginning 16 May 2022 (123).
- Attendances then decreased remaining fairly stable, averaging 83 attendances per week throughout June, July and August 2022.
Update
For the most recent time period (5 September to 27 November 2022):
- 1,022 ED attendances were recorded, an average of 85 per week. This was 3% higher than the previous twelve-week time period - 13 June to 29 August 2022 (990 attendances, average of 83 per week).
- Attendances were slightly lower when comparing to the similar time period in 2021 (1,068 attendances, average of 89 per week) and 8% lower than those in 2020 (1,114 attendances, average of 93 per week).
Additional information
These data are taken from our Accident and Emergency Data Mart.
Diagnosis and reason for attendance can be recorded in a variety of ways, including in free text fields. Therefore, the numbers presented in this report only give a high-level indication of attendances over time.
For more information, or to analyse these data by NHS board, visit the COVID-19 wider impacts dashboard.
Why we use a 3-week moving average
As these data are highly variable over time, a 3-week moving average has been included in the graph to aid interpretation of trends over time.
Drug-related acute hospital admissions
The average weekly number of drug-related hospital admissions were stable between July and September 2022. The total number of admissions in this time period (2,024) was significantly lower than expected, compared to the same time period in 2020 (3,643) and 2021 (3,033) (decreases of 44% and 33% respectively).
Background
The data used in these statistics relate to all inpatient and day case admissions to general acute hospitals (excluding maternity, neonatal, geriatric long stay and admissions to psychiatric hospitals), where drug use was recorded as a diagnosis at some point during the patient’s hospital stay. Data are presented by date of admission.
The chart below shows the weekly number of drug-related admissions to Scotland’s general acute hospitals from 29 June 2020 to 25 September 2022.
Summary
Historic trend
- There was a long-term decreasing trend in the average weekly number of drug-related hospital admissions from June 2021 to April 2022. Admissions briefly increased in April and May 2022, before decreasing again in June 2022.
- The long-term decreasing trend in drug-related hospital admissions observed since June 2021 differs markedly from previous years, which have generally been characterised by lower numbers of admissions during winter months and higher numbers during summer months.
Update
For the most recent time period (27 June to 25 September 2022):
- 2,024 drug-related hospital admissions were recorded, at an average of 155 per week. Weekly numbers of admissions were generally stable throughout this period, ranging from 130 to 180.
- The total number of admissions was lower than expected compared to previous years:
- 44% lower than the same period in 2020 (3,643, at an average of 280 per week); and,
- 33% lower than the same period in 2021 (3,033, at an average of 233 per week).
- The most common substance type recorded in drug-related general acute hospital admissions between July and September 2022 was opioids (47% of admissions).
Additional information
These data have been extracted from our SMR01 dataset.
The data presented on drug type is based on ICD-10 diagnostic codes and is not confirmed by toxicology analysis.
For more information on diagnostic coding, please refer to the drug-related hospital statistics publication methods page.
To analyse the latest published information by NHS Board or by Alcohol and Drug Partnership (ADP), go to our information on drug-related hospital statistics admissions.
Why we use a 3-week moving average
As these data are highly variable over time the 3-week moving average has been included in the graph to account for this variability and provide an average line.
Glossary
- Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids include synthetic (lab-made) drugs such as methadone and buprenorphine, as well as opiates (drugs made from opium) such as heroin and morphine.
Suspected drug deaths
The average weekly number of suspected drug deaths increased in October and November 2022, following a decreasing trend in recent months. There were 76 suspected drug deaths in October 2022 and 109 suspected drug deaths in November 2022. The number of suspected drug deaths in November 2022 (109) was 17% higher than in November 2020 (93) and 22% higher than in November 2021 (89).
Background
Suspected drug death figures are based on reports from police officers attending scenes of death. The details of these events are recorded by Police Scotland and shared with Public Health Scotland.
Following further investigation, these suspected drug deaths are either confirmed as a ‘drug-related death’ or determined ‘not to be a drug death’. This can take several months so suspected figures are used to provide a timely indication of trends and inform prevention activity.
The chart below shows the weekly number of suspected drug deaths in Scotland from 28 June 2020 to 27 November 2022.
Summary
Historic trend
- Following a large increase in suspected drug deaths in Scotland during December 2020, there was a decreasing trend in the average weekly number of deaths until May 2021. The number of suspected drug deaths increased during summer 2021, peaking at 34 in the week beginning 7 June 2021.
- Between July 2021 and June 2022, the average number of suspected drug deaths remained relatively stable, generally ranging between 15 and 25 deaths per week.
Update
For the most recent time period (4 July to 27 November 2022):
- An average of 20 suspected drug deaths were recorded per week (ranging between 12 and 31). This was slightly lower than for the same weeks in 2020 and 2021 (an average of 22 deaths per week in both years).
- There was an increase in the average number of suspected drug deaths per week during October and November 2022. In the week beginning 31 October 2022, there were 31 suspected drug deaths. This was a 72% increase compared to the previous week (18) and the highest weekly total recorded since week beginning 30 May 2022 (32).
Additional information
Data on suspected drug deaths in Scotland are provided by Police Scotland.
Other data on drug deaths are published by the Scottish Government. Quarterly information on Police Scotland suspected drug deaths includes comparisons with National Record of Scotland’s (NRS) National Statistics and provides details on the age, sex and geographical location of suspected drug deaths.
The information above is management information and not subject to the same validation and quality assurance as Official Statistics. National Statistics on drug-related deaths in 2021 and earlier years – broken down by age, sex, substances implicated and NHS Board and council areas – are published annually by the NRS.
The data provided in this release should not be viewed as indicative of the annual deaths reported by NRS.
Detailed information on drug-related deaths is presented in the National Drug-Related Deaths Database, which is published by PHS every two years. The latest report describes deaths that occurred in 2017 and 2018, with trend data from 2009.
Why we use a 3-week moving average
As these data are highly variable over time, a 3-week moving average has been included in the graph to aid interpretation of trends over time.
Glossary
- Drug-related death
A drug-related death (also referred to as drug-misuse death) is a death where the underlying cause was confirmed to be drug poisoning and where any of the substances that were implicated or potentially contributed to the death are controlled in the UK. National Statistics on drug-related deaths are published by NRS. In 2021, there were 1,330 drug-related deaths in Scotland. This was a small decrease compared to 2020 (1,339), which saw the highest annual total on record.
- Suspected drug death
A suspected drug death is a death where controlled drugs are suspected of being involved. This operational measure used by Police Scotland is based on the reports, observations and initial enquiries of officers attending the scene of death.
Toxicology indicators
Emergency department toxicology: ASSIST
Between August and November 2022, 169 detections of 30 different illicit drugs were identified by the ASSIST pilot. More than one substance was detected in 82% of attendances. The most commonly detected drug category was depressants (58%), followed by stimulants (27%). The most commonly detected drug was cocaine (13%), followed by desmethyldiazepam (11%).
Background
The ASSIST (A Surveillance Study in Illicit Substance Toxicity) pilot conducted by the emergency department (ED) at the Queen Elizabeth University Hospital (QEUH) aims to assess the feasibility of prospective surveillance of ED attendances due to acute illicit drug toxicity.
The study collects anonymised data through analysis of standard of care clinical data for severely ill patients attending the ED due to illicit drug toxicity.
The use of the term ‘illicit drug’ encompasses any substance that is controlled. It excludes:
- legal substances such as alcohol, nicotine, caffeine and paracetamol
- medications recently prescribed to the individual
- drugs administered to the individual as part of treatment (by ambulance or hospital)
The pilot enables full toxicological analysis through the biorepository. This allows drug profiling and the identification of emerging drugs or changing trends, to inform appropriate harm reduction measures and public health responses.
This pilot will run in the QEUH ED in Glasgow from August 2022 to August 2023, followed by a three-month follow up period.
Toxicology analysis of surplus serum samples
Surplus serum samples are left over blood samples, that were taken as part of usual care. The chart below shows the most common drug categories detected in toxicology analysis of surplus serum samples between 17 August 2022 and 16 November 2022. The results are shown as the total number of detections, broken down by top five drug categories and then broken down further by drug name.
Summary
For the most recent time period (17 August 2022 to 16 November 2022), 273 discreet ED attendances related to illicit drug use were identified.
Drug type and category
Complete toxicology and clinical data are available for 38 attendances, with results described below. Results from the remaining attendances will be available in the next report.
- There was a total of 169 detections of 30 different illicit drugs found through the biological detection of the drug or its metabolite.
- The following drugs were most commonly detected:
- cocaine: 22 (13%)
- desmethyldiazepam: 17 (10%)
- cannabis: 15 (9%)
- etizolam: 14 (8%)
- temazepam: 14 (8%)
- Depressants were the most common drug category, detected 98 times, making up 58% of all detections.
- Benzodiazepines were detected 88 times (52%). 12 different types of benzodiazepines were detected.
- Gabapentinoids were detected 10 times (6%), three gabapentin and seven pregabalin.
- Stimulants were the second most common drug category, detected 33 times, making up 20% of all detections.
- The most common stimulant was cocaine, detected 22 times (13%).
- There were four detections for amphetamine, three for methamphetamine and two for MDMA. Mephedrone and MDA were each detected once.
- Opioids were the third most common drug category, detected 21 times, making up 12% of all detections.
- Codeine, methadone and dihydrocodeine were each detected four times. Dihydromorphine, buprenorphine and morphine were detected twice. There were two detections of morphine (a metabolite of heroin and other opioids).
Polydrug use
- Polydrug use is a prevailing feature with 31 tests (82%) detecting more than one illicit drug or metabolite, even after legal substances (such as alcohol) and known prescribed medicines (including prescribed benzodiazepines and opioids) are removed.
- The number of illicit drugs detected for each attendance ranged between one and 12, with a mean of four.
- 48% of cases positive for a benzodiazepine also tested positive for an opioid. 100% of cases positive for an opioid also tested positive for a benzodiazepine.
- 59% of cases positive for a benzodiazepine also tested positive for cocaine. 73% of cases positive for cocaine also tested positive for a benzodiazepine.
Further findings
Complete clinical data is available for 134 attendances, with results described below.
- 96 were male (72%) and 38 were female (28%).
- Just over half were 16 to 34 years old.
| Age category | Total | Percentage of total |
| 16 to 24 | 30 | 22% |
| 25 to 34 | 41 | 31% |
| 35 to 44 | 35 | 26% |
| 45 to 54 | 15 | 11% |
| 55 to 74 | 11 | 8% |
| 75 and over | 0 | 0% |
| Unknown | 2 | 1% |
- 109 patients were in hospital for 24 hours or less (81%).
- ED outcome records show that five patients were admitted to an intensive care unit. 24 were admitted to a ward or high dependency unit. 10 were transferred to a psychiatric unit. 75 were discharged home and 20 were recorded as ‘other’ (including discharged to police custody, self-discharge and unknown).
- Clinical severity outcome (after 28 days) recorded that 120 patients recovered and 3 patients died. 11 outcomes were recorded as ‘other’ including ongoing inpatient stay, disabled and unknown.
Additional information
Public Health Scotland (PHS) was provided with these data by QEUH, NHS Greater Glasgow and Clyde (GGC).
The ASSIST trial is registered with Clinical Trials UK (ID: NCT05329142).
Ethical approval has been granted by the West of Scotland Research Ethics Service (IRAS ref: 313616, REC ref: 22/WS/0047) and surplus sampling methodology through Biorepository Ethics (ref: 22/WS/0020).
The West of Scotland Safe Haven research database hosts the electronic clinical data under IRAS ref: 321198 or REC ref: 22/WS/0163.
This study is sponsored by NHS GGC Research and Innovation and is funded by the Scottish Government.
The testing has been carried out by the LGC Group. LGC analyse pseudonymised samples using mass spectrometry and screen against a database of over 3,500 analytes. This testing can detect drugs and metabolites, but this analysis does not imply that specific drugs were implicated in harms.
Further information on the study can be found at Clinical Trials UK.
Glossary
- Depressants
Depressant drugs depress the central nervous system, which also decreases heart rate and breathing. Depressant drugs include substances such as benzodiazepines and gabapentinoids.
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers. Benzodiazepines (and metabolites) detected in this project include desmethyldiazepam, etizolam, temazepam, oxazepam, diazepam, bromazolam, gidazepam, flubromazepam, flualprazolam, lorazepam, nitrazepam and alprazolam. Please note that desmethyldiazepam, temazepam and oxazepam are all benzodiazepine drugs in their own right but can also be found as a metabolite of diazepam.
Gabapentinoids (pregabalin and gabapentin) are a group of drugs with depressant and painkilling effects.
- Stimulants
Stimulant drugs stimulate the central nervous system, which also increases heart rate and breathing. Stimulants drugs include substances such as cocaine and amphetamines.
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing. This group includes powder cocaine and crack cocaine.
Other stimulants are stimulant drugs apart from cocaine. Stimulants detected in this project include amphetamine, methamphetamine, MDMA, mephedrone and MDA.
- Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids detected in this project include codeine, methadone, dihydrocodeine, tramadol, dihydromorphine, buprenorphine and morphine.
- Cannabinoids
Cannabinoids are compounds that interact with the endocannabinoid system. They are found in the cannabis plant (such as THC) or can be produced synthetically in a laboratory (synthetic cannabinoids). No synthetic cannabinoids were detected in this project. All cannabinoid detections are for cannabis.
- Unique ED attendances
In this quarter there was a total of 273 unique attendances to the emergency department related to illicit drug use. Each separate attendance is counted as one. If the same person presented more than once, each attendance would be a separate data point.
- Illicit drug
The use of the term 'illicit drug' encompasses any substance that is controlled. It excludes:
- Legal substances such as alcohol, nicotine, caffeine and paracetamol
- Medications recently prescribed to the individual
- Drugs administered to the individual as part of treatment (by ambulance or hospital)
- Metabolite
A drug metabolite is a compound produced when a drug breaks down in the body.
In this study, if either a drug or metabolite are detected, this will only be included as one substance – the drug. For example, if both diazepam and its metabolite desmethyldiazepam are detected, only diazepam is recorded.
If only a metabolite is detected this will be documented as the substance.
Due to this we are unable to ascertain the source of some substances, for example, oxazepam is a benzodiazepine, but it is also a metabolite of a range of other benzodiazepines, so we cannot determine whether oxazepam or another benzodiazepine was consumed.
Forensic toxicology testing for controlled substances
The total number of deaths testing positive for controlled substances via Forensic Medicine and Science (FMS) toxicology testing was 16% lower in Q3 of 2022 (1 July 2022 to 30 September 2022) than in Q2 (1 April 2022 to 30 June 2022).
In Q3 of 2022, the most commonly found drugs or drug types were opioids (74%) and benzodiazepines (50%). Heroin/morphine was detected in 35% of deaths and there was a continued reduction in detections for etizolam (17%) and methadone (25%).
Background
This analysis is based on toxicology testing data completed at post-mortem.
This testing was performed by the Forensic Toxicology Service based within FMS at the University of Glasgow, on behalf of the Crown Office and Procurator Fiscal Service.
The range of substances routinely analysed by this service is extensive and includes the detection of alcohol, prescribed medicines and controlled drugs.
The first chart below provides an indication of controlled drugs found present at post-mortem in deaths occurring between 1 January 2020 and 30 September 2022.
The second chart provides an indication of specific opioids and benzodiazepines found present at post-mortem in deaths occurring between 1 January 2020 and 30 September 2022.
Summary
Historic trend
- In total, 2,172 deaths occurred in 2021 where controlled drugs were found present via FMS toxicology testing, which was 2% higher than in 2020 (2,136).
- The most commonly found drug types were opioids and benzodiazepines. The percentage of deaths with these drugs present increased during the time period when the initial COVID-19 restrictions were in place (Q2 of 2020) and remained high throughout 2020 to Q2 of 2021, but has been decreasing since Q3 of 2021.
- The specific drugs most commonly present throughout the time series (from Q1 of 2020 to Q2 of 2022) were etizolam, methadone and heroin/morphine, with etizolam and methadone both increasing sharply in Q2 of 2020.
- Although there was a gradual reduction in deaths where methadone was found present, etizolam presence remained high throughout 2020 and early 2021 before sharply decreasing in Q3 of 2021.
- The percentage of deaths involving diazepam, other opioids, gabapentin/ pregabalin or cocaine have remained relatively stable over time.
Update
- The total number of deaths testing positive for controlled substances via FMS toxicology testing was 16% lower in Q3 of 2022 (1 July 2022 to 30 September 2022) than in Q2 (1 April 2022 to 30 June 2022) and 9% lower than in Q3 of 2021.
- In Q3 of 2022, the following drugs or drug types were most commonly detected:
- opioids: 329 (74%)
- benzodiazepines: 221 (50%)
- gabapentin/pregabalin: 152 (34%)
- cocaine: 130 (29%)
- Following a continued reduction in cases testing positive for etizolam (from 35% in Q1 to 17% in Q3) and methadone (from 34% in Q1 to 25% in Q3), the most commonly found substance was heroin/morphine (35% in Q3 of 2022).
- In Q3 of 2022, the percentage of cases testing positive for etizolam fell below diazepam (24% in Q3 of 2022), which remained relatively stable.
- There were no deaths positive for clonazolam via FMS testing in Q3 of 2022, in comparison to a peak of 12% of deaths in Q3 of 2021.
- Other toxicology sources suggest the ‘street’ benzodiazepine market continues to diversify, with substances such as bromazolam increasingly in use. The decrease in benzodiazepine detections described above may be due to these emerging compounds not being included in testing during this time period. These data will develop further as bromazolam (and other new or emerging drugs) are added to toxicology screening in the coming months.
Additional information
PHS was provided with these data by FMS, University of Glasgow.
Detailed interpretation of the levels of drugs found present, drug interactions, co-morbidities or other factors relating to death are outside the scope of this analysis. This analysis does not imply that specific drugs were implicated in deaths nor that deaths were classified as ‘drug-related’ and does not include consideration of wider causes of death.
The data above are for deaths occurring in the west, east and parts of the north of Scotland. Apart from a very small number of cases analysed at the University of Glasgow, post-mortem toxicology testing for deaths occurring in Aberdeen and the far north of Scotland is conducted by a similar service at the Aberdeen Royal Infirmary (ARI). Results from the ARI are not included in the analysis above.
Glossary
- Benzodiazepines
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers.
Diazepam is a ‘prescribable benzodiazepine’.
Etizolam, clonazolam and bromazolam are ‘street benzos’, benzodiazepines that are not licensed for prescription in the UK.
- Cocaine
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing.
This group includes powder cocaine and crack cocaine.
- Gabapentin/pregabalin
Gabapentin and pregabalin are gabapentinoids, a group of drugs with depressant and painkilling effects.
- Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). This category includes buprenorphine, fentanyl, heroin/morphine and methadone.
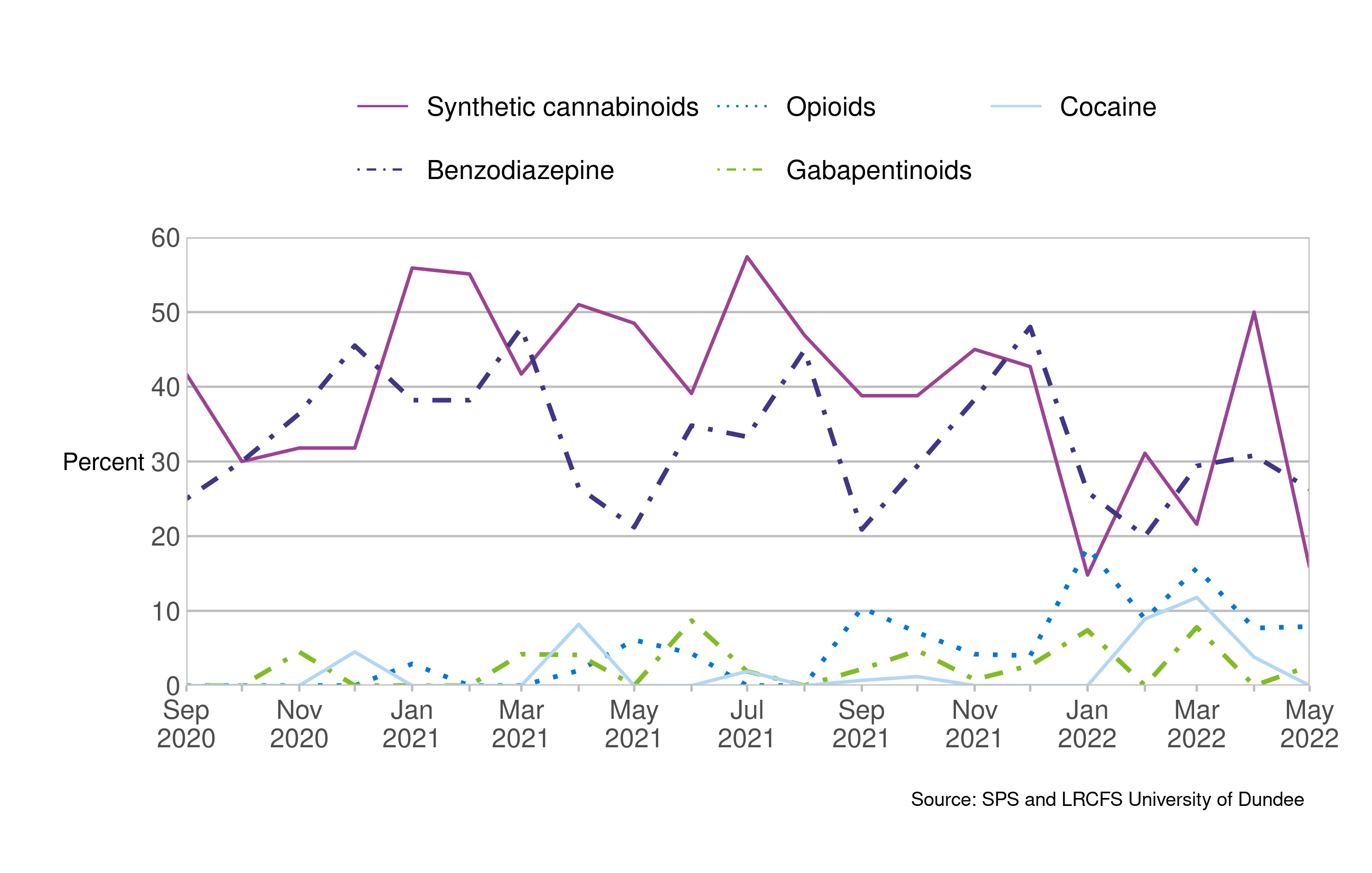
Drug seizures in Scottish prisons
Synthetic cannabinoids were the most prevalent drug type in the Scottish Prisons Non-Judicial Drug Monitoring Project during April, detected in 50% of samples. In contrast, benzodiazepines were the most prevalent in May, detected in 27% of samples.
Background
The Leverhulme Research Centre for Forensic Science (LRCFS) is currently undertaking research with the Scottish Prison Service (SPS). The Scottish Prisons Non-Judicial Drug Monitoring Project tests drug seizures made across the Scottish prison estate in order to understand the changing characteristics of synthetic drugs, including synthetic cannabinoids, often referred to as ‘spice’.
The chart below shows the five drug types most commonly detected in drug seizures in Scottish prisons between 1 September 2020 and 31 May 2022, based on the percentage of all samples tested.
The second chart shows the four sample types most commonly seized in Scottish prisons between 1 September 2020 and 31 May 2022, based on the percentage of all samples tested.
Summary
Historic trend
- Synthetic opioids were the most common substances seized throughout the time series, followed by benzodiazepines. However, both were highly variable over time:
- The percentage of seizures testing positive for synthetic cannabinoids decreased markedly between July 2021 (57%) and January 2022 (15%). Overall, an average of 47% of seizures in 2021 tested positive for synthetic cannabinoids compared with 19% between January and March 2022.
- The percentage of seizures testing positive for benzodiazepines fluctuated throughout 2021 with an average of 45% per month for the year (ranging from 21% to 48%). The percentage then decreased and remained stable from January to March 2022 (average of 22%).
- Opioid detections increased at the start of 2022, averaging 17% per month from January to March 2022 compared to 4% in 2021.
- Paper samples were the most common sample types seized in 2021, accounting for an average of 53% of samples per month. This fell to an average of 26% per month from January to March 2022. Increasing trends in the percentage of powder (average of 17% per month) and tablet (35% per month) samples were observed from January to March 2022.
Update
Please note, that data for the full time period (April to June 2022) were not available. This update provides analysis of samples seized in April and May 2022 (63 samples).
For the most recent time period (1 April 2022 to 31 May 2022):
- The three most commonly detected drugs were ADB-BUTINACA (synthetic cannabinoid), ADB-HEXINACA (synthetic cannabinoid) and etizolam (benzodiazepine).
- Synthetic cannabinoids were the most common drug type, detected in an average of 30% of seizures. This was lower than the same time period in 2021 (50%).
- Benzodiazepines were the second most common drug type, detected in an average of 29% of seizures. This was higher than the same time period in 2021 (24%).
- A continuing increasing trend in the percentage of powder and paper samples was observed in April (39% paper, 38% powder). Paper samples decreased in May (11% compared to a monthly average of 53% in 2022). An increase in tablet samples was also observed (38%).
Further findings
A small number of samples (31) were tested between June and September 2022, with these broadly following previously observed trends. 58% of samples tested positive for synthetic cannabinoids and 32% for benzodiazepines.
Additional information
PHS was provided with these data by SPS and LRCFS.
The Scottish Prisons Non-Judicial Drug Monitoring Project is a collaboration between the SPS and the LRCFS at the University of Dundee.
An initial pilot project ran between September 2018 and January 2021. The project has been directly funded by SPS since February 2021.
Glossary
- Benzodiazepines
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers. Benzodiazepines detected in this project include etizolam, flubromazepam, bromazolam, diazepam and flualprazolam.
- Cocaine
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing. This group includes powder cocaine and crack cocaine.
- Gabapentinoids
Gabapentinoids are a group of drugs with depressant and painkilling effects. On average, in this project 16% of gabapentinoid detections are for gabapentin and 84% are for pregabalin.
- Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids include synthetic (lab-made) drugs such as methadone and opiates (drugs made from opium) such as heroin. Opioids detected in this project include buprenorphine, heroin, tramadol, codeine, dihydrocodeine, metonitazene, oxycodone and methadone.
- Synthetic cannabinoids
'Synthetic cannabinoids' is a term used to describe over 200 lab-made drugs that interact with the endocannabinoid system.
The prevalence of synthetic cannabinoids in seizures is higher in prisons than in the general population.
People working and living in prisons should be aware of the harmful effects and risks of synthetic cannabinoid use.
Visit NHS inform for more information on synthetic cannabinoids.
Service indicators
Specialist drug treatment referrals
The average weekly number of referrals to specialist drug treatment services was stable from August to November 2022. The number of referrals during this time period (4,620) was lower compared to the same time periods in 2020 (5,092) and 2021 (5,511).
Background
Specialist drug treatment referrals occur when a person comes into contact with services designed to support their recovery from problem drug use.
Figures shown are for referrals relating to either drug use or co-dependency (people seeking help for both drug and alcohol use). Figures include new referrals for treatment and referrals between services.
The chart below shows the weekly number of referrals to specialist drug treatment services between 7 August 2020 and 13 November 2022.
Summary
Historic trend
- The average weekly number of referrals increased from September 2020 to May 2021, reaching a peak of 554 in week beginning 17 May 2021.
- Referrals decreased throughout June and July 2021, and then remained stable to January 2022 (between 400-480 referrals per week, apart from the seasonal decrease in December and January).
- From January 2022 onwards, there has been a gradual decrease in the average weekly number of referrals.
Update
For the most recent time period (22 August to 13 November 2022):
- 4,620 specialist drug treatment referrals were recorded, at an average of 385 per week.
- This was almost the same as the previous twelve-week time period (30 May to 21 August 2022) when 4,622 referrals were recorded, at an average of 385 per week.
- Referrals were 9% lower compared to the same time period in 2020 (5,092, at an average of 424 per week) and 16% less than those in 2021 (5,511, at an average of 459 per week).
Additional information
These data are taken from the Drug and Alcohol Information System (DAISy) and its predecessor, the Drug and Alcohol Treatment Waiting Times (DATWT) database.
For more information, or to analyse these data by NHS Board, visit the COVID-19 wider impacts dashboard.
PHS publishes further information on waiting times for people accessing specialist drug and alcohol treatment services. The latest data can be viewed in our National Drug and Alcohol Treatment Waiting Times report.
For details of drug treatment services in your area, visit the Scottish Drug Services Directory.
The Medication Assisted Treatment (MAT) Standards are an improvement programme to strengthen access, choice and support within the drug treatment system in Scotland.
Why we use a 3-week moving average
As these data are highly variable over time, a 3-week moving average has been included in the graph to aid interpretation of trends over time.
Opioid substitution therapy
The average number of OST doses supplied per month decreased slightly in the period from July to September 2022. The number of OST doses supplied during this period was higher than in the same time period in 2018 and 2019, and lower than in the same time period in 2020 and 2021.
Background
The data used in these statistics relate to the number of average daily quantity (ADQ) doses for opioid substitution therapy (OST) drugs dispensed in the community in Scotland. OST drugs include methadone, oral buprenorphine and injectable buprenorphine.
The first chart below shows the average total monthly number of ADQ doses supplied for OST medications in the community between January 2018 and September 2022.
The chart below shows monthly trends in the number of ADQ doses supplied for specific OST medications in the community between January 2018 and September 2022.
Summary
Historic trend
- From early 2018 to early 2020, the average total monthly number of OST doses supplied was broadly stable. In February 2020, the number of OST doses increased, peaking in June 2020. There was a decreasing trend in the average monthly total number of OST doses supplied between July 2020 and June 2022.
- The average monthly number of methadone doses supplied was stable from early 2018 to early 2020, increased between February 2020 and June 2020 and has gradually decreased since then.
- The average monthly number of oral buprenorphine doses supplied increased gradually from early 2018 to June 2020 and has remained broadly stable since.
- Injectable buprenorphine was first licensed for use in Scotland in early 2020. The average total number of doses supplied has increased steadily since then, to approximately 63,000 in June 2022.
Update
For the most recent time period (July to September 2022):
- The average total monthly number of OST doses supplied was approximately 747,800.
- This was roughly the same as in the previous quarter (April to June 2022) when approximately 749,700 doses were supplied.
- The number of OST doses supplied was higher (both 3%) than in July to September in 2018 and 2019 and lower (5% and 3% respectively) than in the same time period in 2020 and 2021.
- The average monthly number of methadone doses supplied was approximately 563,900. Equivalent figures for oral buprenorphine and injectable buprenorphine were 118,300 and 65,700 respectively.
- The number of methadone doses was lower than in the previous quarter (April to June 2022) when approximately 569,000 doses were supplied.
- The number of methadone doses supplied was between 8% and 16% lower than in July to September in previous years (2018 to 2021).
- The number of oral buprenorphine doses supplied was roughly the same as in the previous quarter, higher than the same time period in 2018 and 2019 (21% and 12% higher respectively) and lower than the same time period in 2020 and 2021 (7% and 6% lower respectively).
- The number of injectable buprenorphine doses was 5% higher than in the previous quarter and 44% higher than in the same time period in 2021.
Additional information
These data have been extracted from Prescribing Information System (PIS) and the Hospital Medicines Utilisation Data Manual (HMUD).
The data shown on methadone and oral buprenorphine, and the majority of injectable buprenorphine data, relate to prescriptions dispensed to an individual from a community pharmacy in Scotland where a request for reimbursement of costs was processed. These community prescribing data are extracted from PIS. The time period reflects the month for which reimbursement was claimed. This is regarded as the most comprehensive and reliable way of reporting community prescribing data. There can be a lag of approximately three months from a prescription being written to reimbursed data becoming available.
As a consequence of the direct administration of injectable buprenorphine within clinics, some NHS Boards do not request the reimbursement of costs for all of the OST treatments they provide. Data for approximately 30% of injectable buprenorphine doses supplied in Scotland are held in HMUD and have been combined with the community prescribing data to provide a comprehensive account of OST supply over time.
The time period shown for HMUD data reflects the month in which medication was purchased. For injectable buprenorphine, the length of time between the purchase and administration of medication is thought to be generally short. Therefore, the differences in the basis of the time periods shown in PIS and HMUD data are not thought to negatively impact the reliability of this analysis.
To analyse information on methadone and oral buprenorphine dispensing by NHS Board or by Alcohol and Drug Partnership, go to the COVID-19 wider impacts dashboard.
Why we use a 3-month moving average
As these data are highly variable over time, a 3-month moving average has been included in the charts to aid interpretation of trends over time.
Even if all other factors are constant (for example, the number of treated patients), the total number of ADQ doses supplied will vary according to the number of days in each month. Averaging over three months minimises the impact of that variability.
What is average daily quantity (ADQ)?
When comparing use between medicines and over time, it is common to use World Health Organization (WHO) Defined Daily Doses (DDDs). The DDD is defined as the usual average daily maintenance dose used in adults for the main therapeutic use of the medicine. The WHO DDD is a global average and may not be representative of the doses used in clinical practice at a more local level. This is particularly the case for methadone, where the WHO DDD of 25 milligrams (mg) daily is between one-half and one-third of the normal maintenance dose used in Scotland.
We have therefore replaced DDDs with ADQs, which are more representative of the daily maintenance doses used within Scotland. These values have been developed through a combination of prescription analyses and by consultation with the Specialist Pharmacists in Substance Misuse group. The ADQs agreed are:
- methadone (oral): 65 mg
- buprenorphine (oral): 13 mg
- buprenorphine (parenteral/injectable): 3.4 mg
Glossary
- Methadone
Methadone is an opioid drug commonly prescribed as an opioid substitution therapy. Methadone is a full opioid agonist – it is most commonly seen as a green liquid, which is swallowed. These data refers to methadone prepared as a 1 mg/ml solution.
- Buprenorphine
Buprenorphine is an opioid drug commonly prescribed as an opioid substitution therapy. Buprenorphine is a partial opioid agonist – it is available in oral and injectable forms:
- Oral buprenorphine is buprenorphine in tablet form that is administered orally (by mouth, usually sub-lingual – under the tongue). It is also known by brand names such as Subutex. These data include 2 mg, 8 mg and 16 mg tablets.
- Injectable buprenorphine is buprenorphine in liquid form that is administered as a subcutaneous injection. It is also known by brand names such as Buvidal. These data include various weekly and monthly prolonged release formulations
- Defined daily dose (DDD)
As defined by the World Health Organization, the DDD is ‘the assumed average maintenance dose per day for drug use for its main indication in adults’.
- Average daily quantity (ADQ)
ADQ is similar to the DDD but adjusted to reflect how medication is used in Scotland.
Injecting equipment provision
The average weekly numbers of Injecting Equipment Provision (IEP) transactions and needles and syringes distributed were broadly stable between July and September 2022. The total numbers of IEP transactions and needles and syringes distributed during this time period were lower compared to the same time periods in 2020 and 2021.
Background
IEP is a form of harm reduction that helps to reduce the transmission of blood borne viruses among people who inject drugs. These data relate to the number of needle/syringe transactions at IEP sites and the total number of needles and syringes distributed.
The first chart below shows the weekly number of IEP transactions from 29 June 2020 to 2 October 2022.
The second chart shows the weekly number of needles and syringes distributed from 29 June 2020 to 2 October 2022.
Summary
Historic trend
- There was an overall decrease in the average weekly number of IEP transactions from June 2020 to February 2022. This trend included seasonal fluctuations during December and January each year. Since February 2022, average numbers of IEP transactions have been relatively stable (approximately 3,000 per week).
- A fluctuating decreasing trend in the average weekly number of needles and syringes distributed was observed from June 2020 to July 2021. Since July 2021, the average number distributed has remained relatively stable (approximately 37,500 per week).
Update
For IEP transactions in the most recent time period (4 July 2022 to 2 October 2022):
- 38,644 transactions were recorded, at an average of 2,973 per week.
- This was comparable to the previous time period (4 April to 3 July 2022) when a total of 38,102 were recorded, at an average of 2,931 per week.
- The total number of transactions was 17% lower compared to the same time period in 2020 (46,365, at an average of 3,567 per week), and 15% lower compared to those in 2021 (45,221, at an average of 3,230 per week).
For needles and syringes distributed in the most recent time period (4 July 2022 to 2 October 2022):
- 492,782 needles and syringes were distributed, at an average of 37,906 per week.
- This was comparable to the previous time period (4 April to 3 July 2022) when a total of 483,377 needles and syringes were distributed, at an average of 37,183 per week.
- The total number of needles and syringes distributed in the most recent time period was 14% lower compared to the same time period in 2020 (571,559, at an average of 43,966 per week), and 11% lower compared to those in 2021 (554,021, at an average of 39,573 per week).
Additional information
These data are taken from the Needle Exchange Online 360 database (neo360).
The 11 mainland NHS Boards use neo360 routinely, but due to missing data for part of the time period presented, NHS Highland is excluded from the transaction data, and both NHS Fife and NHS Highland are excluded from the needle and syringe figures.
For more information, or to analyse these data by NHS board, visit the COVID-19 wider impacts dashboard.
For details of injecting equipment providers in your area, visit the Scottish Needle Exchange Directory.
Why we use a 3-week moving average
As these data are highly variable over time, a 3-week moving average has been included in the graph to aid interpretation of trends over time.
Glossary
- Transaction
A transaction is an episode in which a client received equipment relating to an injecting episode (i.e. a barrel and/or fixed needle and syringe). People who inject drugs may attend IEP outlets at any time, whether or not they are undertaking specialist treatment for problematic drug use.
Contact
General enquiries
If you have an enquiry relating to this publication, please email phs.drugsradar@phs.scot.
Reporting a drug harm
To make a report to RADAR and share information such as trends, incidents and harms related to drugs you can either:
Media enquiries
If you have a media enquiry relating to this publication, please contact the Communications and Engagement team.
Requesting other formats and reporting issues
If you require publications or documents in other formats, please email phs.otherformats@phs.scot.
To report any issues with a publication, please email phs.generalpublications@phs.scot.
Further information
RADAR
Find out more about RADAR – Scotland’s drugs early warning system.
View our new A to Z: A guide to common drug names in Scotland.
Data and intelligence
View our wider drug data and intelligence.
Public health information
Visit Scottish Public Health Observatory (ScotPHO) for further drug-related public health information.
Metadata
The metadata for this document has been split into sections as there are some differences between the indicators.
Police Scotland drug trends bulletin
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides a summary of the drug trend bulletin from Police Scotland Statement of Opinion (STOP) Unit (drugs expertise unit).
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Police Scotland STOP unit
Date that data are acquired
4 January 2023
Release date
24 January 2023
Frequency
Quarterly
Continuity of data
The Police Scotland drug trend bulletins are designed to provide drug trend information, highlighting some of the current trends identified by the police in Scotland and other parts of the UK. The bulletin has and will evolves through time to provide timely distribution of drug related information.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Benzodiazepines are depressant drugs with sedative and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers.
Nitazenes are a group of drugs with depressant and painkilling effects, also known as 2-benzyl benzimidazole opioids.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
The Police Scotland drug trend bulletin highlights some of the current trends identified by the police in Scotland and other parts of the UK.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Police seizures positive for controlled substances displayed as drug type.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Naloxone administration by Scottish Ambulance Service
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on emergency naloxone administration in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Scottish Ambulance Service (SAS)
Date that data are acquired
4 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
31 August 2020 to 27 November 2022, two months in arrears.
Continuity of data
SAS clinicians have been administering naloxone directly to patients experiencing symptoms of an opioid overdose since around 1998. There have been no changes in the guidance given to SAS clinicians regarding the administration of naloxone nor in the recording mechanisms or processes over the time series shown in the analysis. Further details can be found in the substance use section of the COVID wider impacts dashboard.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Naloxone is a medicine used to prevent fatal opioid overdoses. Opioid overdoses are commonly associated with drug-related deaths. These data on the numbers of incidents in which naloxone was administered by SAS clinicians provide an indication of numbers of suspected opioid overdoses.
A small percentage of these administrations will have been due to circumstances other than an illicit opioid overdose (for example, some may relate to prescribed opioid overdoses or to adverse reactions associated with medications administered in the course of emergency treatment).
Also, in a small number of cases, naloxone may be administered to someone who is unconscious for unconfirmed reasons, which may be confirmed at a later point not to have been an opioid overdose. While these data count multiple overdose patients at the same incident separately, multiple naloxone administrations to the same patient at the same incident are not counted separately.
Under some circumstances, naloxone administration will not successfully reverse an opioid overdose (for example, if administered too late) and these statistics should not be interpreted as equating to numbers of lives saved.
Further details can be found in the substance use section of the COVID wider impacts dashboard.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
SAS data on numbers of naloxone incidents are collated from data entered by ambulance clinicians recording medications administered to patients via an electronic tablet in the vehicle. Data recording is typically completed within 30 minutes of the end of an incident. Further details can be found in the substance use section of the COVID wider impacts dashboard.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of incidents in which naloxone was administered by SAS clinicians and moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Drug-related attendances at emergency departments
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on drug overdose or intoxication attendances at emergency departments in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Public Health Scotland – Accident & Emergency Datamart
Date that data are acquired
5 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness 6 July 2020 and 27 November 2022.
Data are available for analysis approximately two months after the events described.
Continuity of data
There have been no changes in the national recording mechanisms or processes over the time series shown in the analysis.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
A drug–related emergency department (ED) attendance is an attendance for a drug intoxication or overdose, either alone, or combined with alcohol intoxication.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
It is not possible to accurately report total attendances for specific conditions using the national A&E dataset, due to the quality of the data available. Diagnosis/reason for attendance can be recorded in a variety of ways, including in free text fields and not all NHS boards submit this information. The numbers presented in this report therefore only give a high–level indication of attendances over time. Further details can be found in the data management – hospital activity webpage.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of drug overdose or intoxication attendances at emergency departments and moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Drug-related acute hospital admissions
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on drug-related acute hospital admissions in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Public Health Scotland – general acute inpatient/day case records (SMR01)
Date that data are acquired
16 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
29 June 2020 and 25 September 2022.
Data are available for analysis approximately two months after the events described.
Continuity of data
There have been no changes in the recording mechanisms or processes over the time series shown in the analysis. Further detail can be found in the drug-related hospital statistics publication background information.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids include synthetic (lab-made) drugs such as methadone and buprenorphine, as well as opiates (drugs made from opium) such as heroin and morphine.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
The data is routinely drawn from hospital administrative systems and International Classification of Diseases 10th Revision (ICD10) Diagnosis Codes used to identify admissions related to drug use. Some caution is necessary when using these data as drug use may only be suspected and may not always be recorded by the hospital. Further details can be found in the PHS drug-related hospital statistics report, and information on hospital administrative systems (SMR) data completeness can be found on the SMR completeness webpage.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of inpatient and day case admissions to general acute hospitals (excluding maternity, neonatal, geriatric long stay and admissions to psychiatric hospitals), presented by month of admission with moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Suspected drug deaths
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on suspected drug deaths in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Police Scotland
Date that data are acquired
14 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
28 June 2020 to 27 November 2022, approximately two months in arrears.
Continuity of data
There have been no changes in the national Police Scotland recording mechanisms or processes over the time series shown in the analysis.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
A sentence providing October 2022 figures was added to the suspected drug deaths headline on 26 January 2023.
Concepts and definitions
Drug-related death
A drug-related death (also referred to as drug misuse death) is a death where the underlying cause was confirmed to be drug poisoning and where any of the substances which were implicated, or potentially contributed to death, are controlled in the UK. National Statistics on drug-related deaths are published by NRS. In 2021 there were 1,330 drug-related deaths in Scotland. This was a small decrease compared to 2020 (1,339), which saw the highest annual total on record.
Suspected drug death
A suspected drug death is a death where controlled drugs are suspected of being involved. This operational measure used by Police Scotland is based on the reports, observations and initial enquiries of officers attending the scene of death.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
This indicator includes data on suspected drug deaths as recorded by all Police Scotland Divisions across Scotland.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Numbers of suspected drug deaths in Scotland and moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
First publication in this series
Next published
25 April 2023
Date of first publication
24 January 2023
Help email
Date form completed
9 January 2023
Emergency department toxicology: ASSIST
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on number of attendances, length of stay and toxicology of presentations due to acute illicit drug toxicity at the Queen Elizabeth University Hospital (QEUH) emergency department (ED), Glasgow, Scotland. This study assesses the feasibility of prospective surveillance of ED presentations due to acute illicit drug toxicity.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
QEUH, NHS Greater Glasgow and Clyde
Date that data are acquired
13 January 2023
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
19 August 2022 to 16 November 2022
Continuity of data
ASSIST: A Surveillance Study in Illicit Substance Toxicity is a pilot by the ED at the QEUH. It will run from August 2022 to August 2023, followed by a three-month follow up period.
QEUH will provide Public Health Scotland with toxicology screening data on a quarterly and ad-hoc basis for the purposes of public health surveillance.
Because the sample size is small, some of the variables are combined in a different way to the data shared in quarterly report 1 (October 2022), to ensure that they are completely non-identifiable. Later outputs may have narrower categories as the numbers become greater.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Unique ED attendances
In this quarter there was a total of 273 unique attendances to the ED related to illicit drug use. Each separate attendance is counted as one. If the same person presented more than once, each attendance would be a separate data point.
Illicit drug
The use of the term ‘illicit drug’ encompasses any substance that is controlled. It excludes:
- legal substances such as alcohol, nicotine, caffeine and paracetamol
- medications recently prescribed to the individual
- drugs administered to the individual as part of treatment (by ambulance or hospital)
Metabolite
A drug metabolite is a compound produced when a drug breaks down in the body.
In this study, if either a drug or metabolite are detected, this will only be included as one substance – the drug. For example, if both diazepam and its metabolite desmethyldiazepam are detected, only diazepam is recorded.
If only a metabolite is detected this will be documented as the substance.
Due to this we are unable to ascertain the source of some substances, for example, oxazepam is a benzodiazepine, but it is also a metabolite of a range of other benzodiazepines, so we cannot determine whether oxazepam or another benzodiazepine was consumed.
Benzodiazepines
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers.
Cocaine
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing.
Gabapentinoids
Gabapentinoids are a group of drugs with depressant and painkilling effects.
Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing).
Cannabinoids
Cannabinoids are compounds that interact with the endocannabinoid system. They are found in the cannabis plant (such as THC) or can be produced synthetically in a laboratory (synthetic cannabinoids).
Other stimulants
Other stimulants are stimulant drugs apart from cocaine. They increase heart rate, breathing and energy.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
Not all data identified for all ED attendances is available for analysis, due to the time required to send and receive toxicology results and to link patient and clinical data.
For quarter 1 of this study:
- total recruited (unique ED attendances related to illicit drug use): 273
- completed Castor (clinical notes made by research nurses) data available: 134
- completed West of Scotland Safe Haven (electronic clinical record) data available: 113
- toxicology results available: 76
- toxicology results presented here (as have corresponding Castor data): 38
The testing has been carried out by the LGC Group. LGC analyse pseudonymised samples using mass spectrometry and screen against a database of over 3,500 analytes including illicit drugs, novel psychoactive substances, synthetic cannabinoid receptor agonists, benzodiazepines and medications. We are confident that the compound screen used by LGC is up to date with known drugs and metabolites so will be detected in this study. This analysis does not, however, imply that specific drugs were implicated in harms.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of ED attendances related to illicit drug use, destination on discharge from the ED, number of hours in the ED, number of hours in hospital, anonymised toxicology results of surplus serum sampling by drug type and drug category.
This study includes patients aged 16 or over attending QEUH adult ED directly related to acute illicit drug use. It excludes patients where the condition is more likely due to a cause other than acute illicit drug use, due to withdrawal, primarily related to alcohol use or where the attendance is due to a complication of previous drug use, i.e. infected injection site.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
16 January 2023
Forensic toxicology testing for controlled substances
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on forensic toxicology testing for controlled substances completed at post-mortem in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Forensic Toxicology Service within Forensic Medicine and Science, University of Glasgow, on behalf of the Crown Office and Procurator Fiscal Service.
Date that data are acquired
19 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
1 January 2020 and 30 September 2022, approximately three months in arrears.
Continuity of data
There have been no changes in the national recording mechanisms or processes over the time series shown in the analysis.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Forensic Medicine and Science undertakes toxicology testing on behalf of the Crown Office and Procurator Fiscal Service for post-mortem cases where controlled drugs (as defined in the Misuse of Drugs Act 1971) were found present.
Detailed interpretation of the levels of drugs found present, drug interactions, co–morbidities or other factors relating to death are outside the scope of this analysis.
This analysis does not imply that specific drugs were implicated in deaths nor that deaths were classified as 'drug–related' and does not include consideration of wider causes of death.
Benzodiazepines
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers. Diazepam is a ‘prescribable benzodiazepine’. Etizolam, clonazolam and bromazolam are ‘street benzos’, benzodiazepines that are not licensed for prescription in the UK.
Cocaine
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing. This group includes powder cocaine and crack cocaine.
Gabapentin/pregabalin
Gabapentin and pregabalin are gabapentinoids, a group of drugs with depressant and painkilling effects.
Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). This category includes buprenorphine, fentanyl, heroin/morphine and methadone.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
The data above are for deaths occurring in the west, east and parts of the north of Scotland. Apart from a very small number of cases analysed at the University of Glasgow, post–mortem toxicology testing for deaths occurring in Aberdeen and the far north of Scotland is conducted by a similar service at the Aberdeen Royal Infirmary (ARI). Results from the ARI are not included in this report.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number and percentage of forensic toxicology cases testing positive for controlled substances by drug type.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Drug seizures in Scottish prisons
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on drug types most commonly detected in drug seizures in Scottish prisons.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Scottish Prison Service (SPS) and the Leverhulme Research Centre for Forensic Science (LRCFS), University of Dundee.
Date that data are acquired
11 October 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
1 March 2020 and 31 May 2022, approximately six months in arrears.
Continuity of data
There have been no changes in the seizures recording mechanisms or processes over the time series shown in the analysis.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Benzodiazepines
Benzodiazepines are a group of drugs with depressant and anxiolytic (anti-anxiety) effects. They are also known as tranquilisers. Benzodiazepines detected in this project include etizolam, flubromazepam, bromazolam, diazepam and flualprazolam.
Cocaine
Cocaine is a short-lasting stimulant drug that increases heart rate and breathing. This group includes powder cocaine and crack cocaine.
Gabapentinoids
Gabapentinoids are a group of drugs with depressant and painkilling effects. On average, in this project 16% of gabapentinoid detections are for gabapentin and 84% are for pregabalin.
Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids include synthetic (lab-made) drugs such as methadone and opiates (drugs made from opium) such as heroin. Opioids detected in this project include buprenorphine, heroin, tramadol, codeine, dihydrocodeine, metonitazene, oxycodone and methadone.
Synthetic cannabinoids
'Synthetic cannabinoids' is a term used to describe over 200 lab-made drugs that interact with the endocannabinoid system.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
Our analysis includes all data provided to PHS by LCRFS. LCRFS does not analysis all seizures from SPS and this data should be considered as a sizeable subset of all national prison seizures.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Percentage of drug seizures analysed by the LRCFS by drug type and sample type (card, paper, powder or tablet).
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Specialist drug treatment referrals
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on specialist drug treatment referrals in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Public Health Scotland – Drug and Alcohol Information System (DAISy)
Public Health Scotland – Drug and Alcohol Treatment Waiting Times Database (DATWT)
Date that data are acquired
29 November 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
7 August 2020 to 13 November 2022, approximately two months in arrears.
Continuity of data
These data have been extracted from Drug and Alcohol Information System (DAISy) and its predecessor, the Drug and Alcohol Treatment Waiting Times (DATWT) database (both Public Health Scotland). DAISy was available in all NHS Boards from April 2021 (while four NHS Boards were early adopters and transferred to DAISy on 1 December 2020; NHS Ayrshire & Arran, NHS Dumfries & Galloway, NHS Grampian and NHS Western Isles).
Direct comparisons between recent and earlier numbers of referrals recorded in DAISy and the DATWT database respectively, should be interpreted carefully (see revisions statement for further explanation).
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
A new continuation of care process was introduced in DAISy which affects how referrals are recorded when people have started treatment and move from one service to another without a break or change in their treatment (for instance, when moving between community-based and prison-based services). Previously in the DATWT database, a referral would have been recorded at both the transferring and receiving service, and the subsequent waiting time for treatment would be recorded at both. In DAISy, if a person is transferred following the continuation of care process, only one wait is recorded, associated with the initial service where the person started treatment, but a referral is recorded for both services. In previous versions of this report these continuation of care referrals were not included. They have been incorporated to improve comparability between DATWT and DAISy.
Revisions relevant to this publication
N/A
Concepts and definitions
These data relate to the number of referrals to specialist drug and alcohol treatment services in Scotland delivering tier 3 and 4 interventions (community-based specialised drug assessment and co-ordinated care-planned treatment, and residential specialised drug treatment). These data are for community-based drug and alcohol treatment services and exclude prison-based services.
An additional ‘co-dependency’ client type was introduced, where the referral relates to treatment for both drug and alcohol use. Co-dependency has only been recorded in all NHS Boards since the introduction of DAISy (April 2021) so is not available as a separate client type in the earlier years. This data is the number of referrals where the client type is recorded as either ‘drugs’ or ‘co-dependency’.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
Drug and alcohol treatment services are required to submit accurate and up-to-date waiting times information to PHS. These referrals data are management information and includes all services that enter data on DAISy and its predecessor, the DATWT database. (This contrasts with the figures reported in the National Drug and Alcohol Treatment Waiting Times Statistics release for Scotland where data from services that were unable to confirm their data were accurate and up-to-date within specified timescales are excluded). Further details can be found in the substance use section of the COVID wider impacts dashboard.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of specialist drug treatment referrals and moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Opioid substitution therapy
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on opioid substitution therapy prescribing in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Public Health Scotland – Prescribing Information System (PIS)
Public Health Scotland - Hospital Medicines Utilisation Database (HMUD)
Date that data are acquired
16 December 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
1 January 2018 to 30 September 2022.
Data from PIS are available for analysis approximately three months after an OST prescription has been dispensed.
HMUD data availability can vary by NHS Board. However, the injectable buprenorphine data shown in this release are considered complete.
Continuity of data
The data shown are considered to provide a comprehensive account of OST prescribing for the time series presented, including data from GP and hospital prescribing systems.
Revisions statement
Data are provisional and may be subject to revision. The data shown in the most recent quarterly update supersedes data reported in previous releases.
Revisions relevant to this publication
N/A
Concepts and definitions
Defined daily dose
When comparing use between medicines and over time it is common to use World Health Organization (WHO) defined daily doses (DDDs). The DDD is defined as the usual average daily maintenance dose used in adults for the main therapeutic use of the medicine. The WHO DDD is a global average and may not be representative of the doses used in clinical practice at a more local level.
Average daily quantity
Due to differences between the average OST doses used in Scotland and the rest of the world, the analysis presented here is based on average daily quantities (ADQs). These are more representative of the daily maintenance doses used within Scotland and were developed via analysis of prescriptions and by consultation with the Specialist Pharmacists in Substance Misuse group. The ADQs agreed are:
- methadone (oral): 65 mg
- buprenorphine (oral): 13 mg
- buprenorphine (parenteral/injectable): 3.4 mg
Buprenorphine
Buprenorphine is a synthetic partial opioid agonist used to treat acute pain, chronic pain and opioid dependence. Prescribed for daily use (oral) or weekly or monthly prolonged release (injectable), buprenorphine relieves opioid cravings and withdrawal symptoms and blocks the effects of other opioids. As with other opioids, buprenorphine can result in sedation, respiratory depression and death. These statistics relate to the prescribing of oral (2 mg, 8 mg and 16 mg buprenorphine or buprenorphine and naloxone tablets) and injectable buprenorphine (various strengths) for the treatment of opioid dependence.
Opioids
Opioid drugs act on opioid receptors to produce sedative and painkilling effects. They are respiratory depressants (reduce heart rate and breathing). Opioids include synthetic (lab-made) drugs such as methadone and buprenorphine, as well as opiates (drugs made from opium) such as heroin and morphine.
Methadone
Methadone is a synthetic opioid agonist used to treat chronic pain and opioid dependence. Prescribed for daily use, methadone relieves opioid cravings and withdrawal symptoms. As with other opioids, methadone can result in sedation, respiratory depression and death. These statistics include data on the prescribing of methadone 1mg/1ml solution for the treatment of opioid dependence.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available are published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
There are differences between community prescribing data (PIS) and hospital prescribing data (HMUD) in the way that dates are allocated to medications supplied. The basis for date allocation in PIS data is the month in which the costs associated with dispensing medication are reimbursed. The basis for date allocation in HMUD data is the month in which medications are supplied for onward administration to patients. While useful to note, these differences are not thought to have a significant impact on the reliability of this analysis.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
The data shown are considered to provide a comprehensive account of OST prescribing for the time series presented, including data from GP and hospital prescribing systems.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Total number of ADQ doses of methadone, oral buprenorphine and injectable buprenorphine supplied in Scotland, based on community and hospital prescribing data.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023
Injecting equipment provision
Publication title
Rapid Action Drug Alerts and Response (RADAR) quarterly report – January 2023
Description
This indicator provides information on injecting equipment provision (IEP) in Scotland.
Theme
Substance use surveillance
Topic
Drugs
Format
HTML
Data source(s)
Public Health Scotland – Needle Exchange Online (neo360)
Date that data are acquired
28 November 2022
Release date
24 January 2023
Frequency
Quarterly
Timeframe of data and timeliness
29 June 2020 to 2 October 2022.
Data are available for analysis approximately three months after the events described.
Continuity of data
Caution is recommended when interpreting these statistics. Service provision in some areas has changed over time. Some outlets will have closed, and others will have opened.
The methods used by areas to count or estimate some of the figures may also have changed.
Revisions statement
Data in the most recent quarterly updates supersedes data reported in previous reports.
Revisions relevant to this publication
N/A
Concepts and definitions
Transactions
Refers to an attendance at an injecting equipment provider, either pharmacy or agency which involved provision of a syringe or needle at IEP outlets. People who inject drugs may attend IEP outlets at any time, whether or not they are undertaking specialist treatment for problematic drug use.
Further details can be found in the PHS Injecting Equipment Provision in Scotland report.
Relevance and key uses of the statistics
Data are collected as part of public health surveillance on substance use in Scotland.
The most up–to–date data available is published in this report to provide a timely indicator of drug trends as part of RADAR, Scotland’s Drugs Early Warning System.
Accuracy
The data are considered accurate.
Data are validated locally by data suppliers/partnerships/sources and checked by PHS.
Where relevant, data quality and completeness issues are described in the text associated with each indicator.
The Code of Practice for Statistics has been followed to ensure a high standard of data value, trustworthiness and quality.
Completeness
This indicator includes data on transactions and needle and syringe distribution by injecting equipment providers in mainland Scotland NHS Boards.
It does not include data for NHS Shetland, NHS Orkney and NHS Western Isles.
The 11 mainland NHS Boards use neo360 routinely, but due to missing data for part of the time period presented, NHS Highland is excluded from the transaction data, and both NHS Fife and NHS Highland are excluded from the needle and syringe figures.
Comparability
Data are not comparable outwith Scotland.
Accessibility
It is the policy of PHS to make its websites and products accessible according to our accessibility statement. Graphs and tables have been assessed against PHS accessibility standards.
Accessibility of the report and findings are of continuous consideration throughout the report development.
Coherence and clarity
The report is available as HTML web pages.
Wherever possible, plain English descriptions have been used within the narrative and any technical words or phrases explained.
Value type and unit of measurement
Number of IEP transactions, number of needles and syringes distributed and moving averages.
Disclosure
Our protocol on statistical disclosure is followed.
Official Statistics designation
Management Information Report
UK Statistics Authority Assessment
N/A
Last published
11 October 2022
Next published
25 April 2023
Date of first publication
11 October 2022
Help email
Date form completed
9 January 2023